Introduction
Physiotherapy in Toronto for Osteoarthritis
Welcome to PhysioExcellence's patient resource about Osteoarthritis.
Osteoarthritis (OA) is the most common form of arthritis. In fact, more than 75 percent of people older than fifty-five show the joint deformations of OA on X-rays. But most of these people have no symptoms. For people who do have the joint pain and stiffness of OA, it can become a crippling disease. Some people suffer from OA in just one joint, while others have it in several joints. It affects more women than men, and most OA patients are over 45.
This guide will help you understand:
- how OA develops
- how doctors diagnose the condition
- what can be done for OA
#testimonialslist|kind:all|display:slider|orderby:type|filter_utags_names:Arthritis|limit:15|heading:Hear from some of our patients who we treated for *Arthritis*#
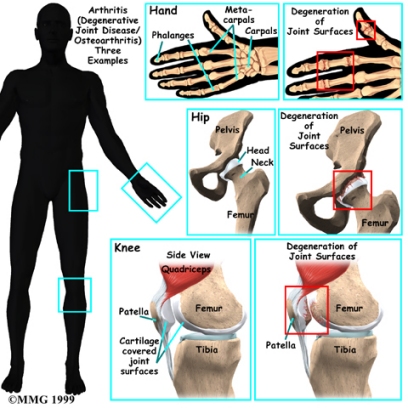
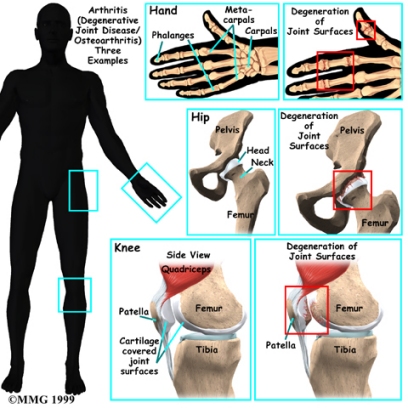
Anatomy
Where does OA develop?
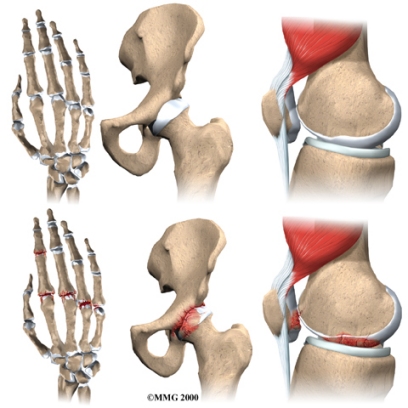
OA is most common in the small joints of the hands, the spine, the knees, the hips, and certain toe joints. OA primarily affects the articular cartilage, the slippery, cushioned surface that covers the ends of the bones in most joints and lets the bones slide without rubbing. Articular cartilage also functions as a shock absorber.
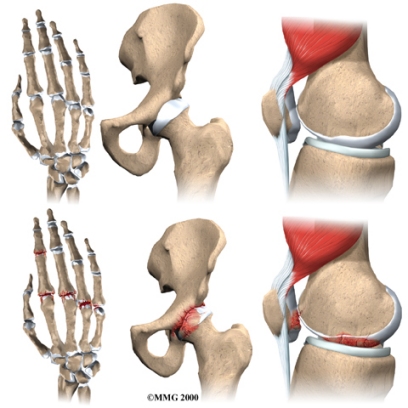
In OA, the articular cartilage becomes damaged or worn away. As this happens, the joint no longer fits together well or moves smoothly. In the early stages of OA, the cartilage actually becomes thicker as your body tries to repair the damage. The repaired areas are more brittle than the original cartilage, and these brittle areas begin to wear away and become thin. They may even wear away entirely. This eventually leads to a condition called eburnation, in which the bones become thick and polished as they rub together. X-rays can show these changes in the cartilage and bones.
But OA is not just a disease of the cartilage. The damage to the cartilage seems to start a sort of chain reaction that involves all the parts of the joint. Bone spurs, or outgrowths, often begin to form around the edges of the joint. The joint capsule (the watertight sack around the joint) can become thickened and lose its stretch. The synovial membrane that lines the inside of the joint capsule may become inflamed (swollen, red, hot, and painful), and crystals may form in the synovial fluid. The tendons and ligaments around the joint can also become inflamed.
Even the muscles around the joint can lose their strength. This usually occurs as a result of under-use of the muscles due to pain in the joint. When something hurts we subconsciously change the way we use the joint to avoid the pain. This causes the muscles to become weakened. Cartilage itself does not have nerves to feel pain, therefore the pain of OA probably comes from these other changes in and around the joint.
Causes
Why do I have this problem?
The exact cause of OA is not known. There are probably different causes in different people. Doctors think of OA in two different categories, primary OA and secondary OA. Primary OA refers to breakdown of a joint from a disease process. Secondary OA means that something else was wrong--an infection in the joint or a fracture for instance--that caused damage to the joint. Even when the original problem clears up, the chain reaction effect of OA can cause the disease to progress.
Major injuries and repetitive stress both seem to cause OA. A person who breaks an ankle is likely to develop OA in that same ankle. Just like any machine, a joint that is damaged and unbalanced wears out faster. People who consistently put heavy stress on the same joint, such as jackhammer operators or baseball pitchers, are more likely to develop OA in that joint.
OA of the knee and hip occurs much more often in people who are seriously overweight. A study that followed overweight young adults for thirty-six years found that being overweight at a young age was closely related to developing OA later in life. The same study also showed that losing even small amounts of weight decreased the odds of developing OA.
Heredity--your genes--may also play a role for some people, especially women. OA in the fingers, which affects ten times more women than men, shows up much more often among women in the same family. Researchers do know that some genes cause problems with cartilage formation.
In some cases, rare metabolic disorders or other problems with the bones or joints can lead to OA. But the primary factor in most patients with OA seems to be age. If you're lucky enough to live a long life, you are much more likely to develop OA.
Symptoms
What does OA feel like?
Patients with OA have one or more joints that are painful and stiff. The pain is a deep, dull ache that usually comes on gradually. Pain gets worse when the joint is used and gets better with rest. The joint is stiff after waking up or after not being used for some time, but the stiffness usually goes away fairly quickly. Over time the pain and the stiffness become almost constant.
No matter which joints are affected, OA patients report many of the same symptoms
- Most patients say that the pain is worse in cool, damp weather.
- Many OA patients feel or hear crackling or popping in the affected joints (called crepitus). This is most common in the knees.
- Joints enlarge or change shape. The enlarged areas are often tender to the touch.
- In most cases the affected joints can't move through a normal range of motion.
- In other cases the joints have become so unstable that they can actually move too much or in the wrong direction.
Some symptoms depend on the affected joint. Patients with knee OA may have problems with the joint locking up, especially when they are stepping up or down. Patients with OA of the hip often limp. OA of the hands can affect the strength and movement of fingers and make simple tasks such as getting dressed very difficult. OA of the spine can cause neck and low back pain as well as weakness and numbness.
Diagnosis
How is the condition diagnosed?
It may seem that diagnosing OA would simply involve a few X-rays. However, it is very important that we rule out other forms of arthritis or causes of joint pain. We will also need to figure out if your OA was caused by another problem or injury (secondary OA). Even if OA is the main problem, the breakdown of cartilage may have caused problems in other parts of the joint that need to be addressed.
Both your physiotherapist and physician will ask you many detailed questions about your health and activity history. Explaining the nature of your pain will be important. Following the history the we will thoroughly examine the affected joints, look at your posture, assess your muscle balance and strength and determine your level of functioning in daily activities. This will help us determine if your pain is stemming from the joints themselves or some other area or cause within the body. X-rays will most likely be taken by your physician. Blood samples and samples of the synovial fluid in the joint may also be taken to try to identify other systemic or inflammatory problems.
Our Treatment
What can be done for the problem?
There is no cure for OA. It is a chronic but very treatable disease. Our goals of treatment at PhysioExcellence are to relieve your pain and to improve or maintain the movement of your joints.
Much of the treatment for OA involves no prescriptions at all. The physiotherapists at PhysioExcellence will encourage you to take several steps to help manage your symptoms:
- Get aerobic exercise.
- Do strengthening and range of motion exercises. These are most often taught and monitored by physical or occupational therapists.
- Lose weight if necessary
- Use heat and/or cold packs.
- Tape the knee, if it is affected.
- Wear insoles in your shoes if the lower extremity is affected.
- Receive massage.
- Use adaptive equipment to help take pressure off your joints, such as a cane or special gadget to open jars.
- Participate in education programs or support groups.
Drugs are available to help alleviate your pain. An over-the-counter pain reliever, such as acetaminophen (Tylenol) may be recommended by your doctor. If this doesn't work, nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen and aspirin, may be prescribed. The main problem with NSAIDs is that they can be very hard on your stomach and kidneys over time and you may be taking these drugs for many years. In rare cases of extreme pain, your physician may prescribe stronger pain medications but these can be addictive and must be used with caution.
All these medications can interact with other drugs. You must let your doctor know what other medicines you are taking, and you must work closely with your doctor to set up dose amounts and schedules.
In recent years, two unique compounds have been used by people with OA. These compounds are gaining greater acceptance among many health care providers. Glucosamine and chondroitin sulfate are dietary supplements taken in pill form that have shown benfits of reducing pain and increasing joint mobility. These treatments are controversial, yet some medical professionals feel there are enough benefits to encourage their patients to supplement with these compounds.
PhysioExcellence provides physiotherapy in Toronto.
Surgery
When pain cannot be relieved and joint function cannot be maintained, your doctor may recommend surgery. While this option may sound scary, surgery can be very effective in treating OA.
Many types of surgical procedures have been designed to treat OA of different joints. Perhaps the most well known treatment is artificial joint replacement. Artificial joint replacement is the final answer to OA after the joint is totally destroyed, but other surgical procedures have been designed to treat osteoarthritis in early stages to reduce symptoms and slow the progression of the disease.
It will take some work to manage your OA, but it is possible. OA doesn't always worsen over time. In many patients the disease stabilizes. In some patients, especially those with OA of the knee, the disease can actually reverse itself. And even when the OA does continue to progress, it often moves very slowly.
Portions of this document copyright MMG, LLC.